This month’s blog spotlights Timothy Dang, an oncodermatologist who is at the forefront of clinicians specializing in patient care during cancer therapy, without being oncologists themselves. The creation of this specialty and its integration into cancer centers highlight a growing emphasis on enhancing the quality of life for those diagnosed with cancer.
What is oncodermatology?
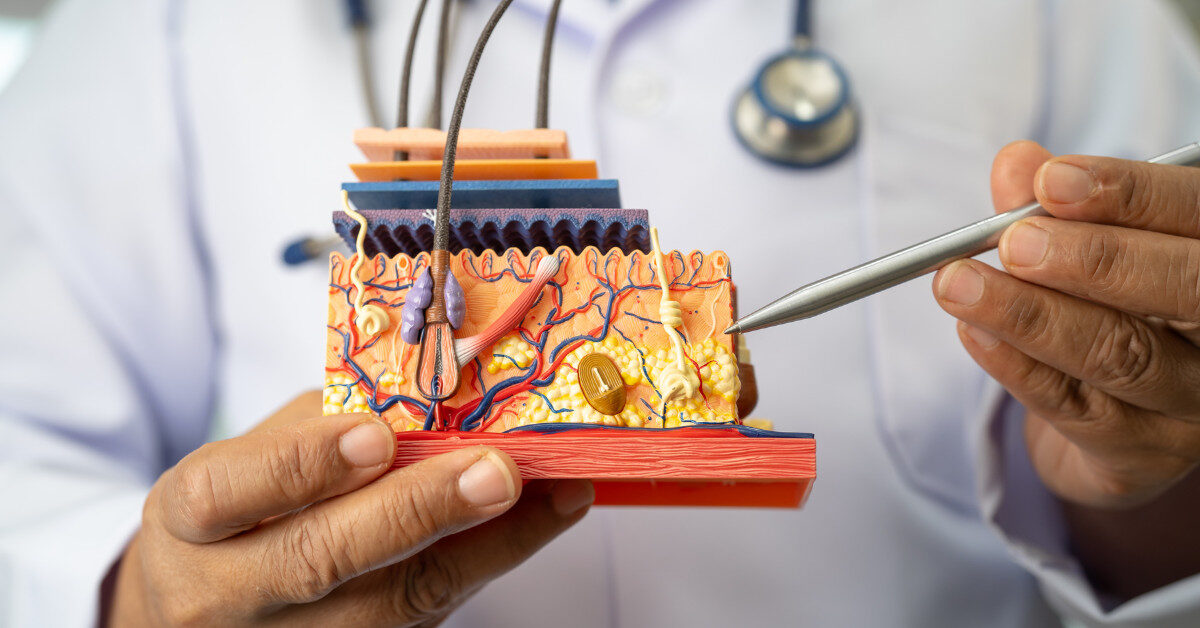
Oncodermatology is a recently described subspecialty within dermatology. Its purpose is to manage the skin of patients undergoing cancer therapy. Our job is to use dermatology’s expertise to help patients better tolerate their therapies and take better care of their skin during therapy.
Why is oncodermatology necessary?
When undergoing cancer treatment, a lot of the side effects of cancer therapy end up affecting the skin, the hair, and the nails. Those side effects are often visible issues that can affect quality of life and function. The reasons why we care about this are two-fold. First, we want to make sure that we are preserving patients’ quality of life, which means that we are helping them feel like themselves while undergoing therapy. Second, we want to ensure we preserve function. For example, we want to help patients address side effects that affect their hands and feet so they can still able to do what they want to do without having their skin be a barrier to those functions.
Therapy reactions can come from chemotherapy, radiation, targeted therapies, and immunotherapies. Those skin reactions can be mild reactions, like eczema, or very severe reactions that require them to stop their cancer therapy. If we effectively take care of these patients, then that prevents patients from needing to reduce a dose of cancer therapy or interrupt their cancer therapy.
What is the biggest misconception about oncodermatology that you hear?
The biggest misconception within the medical field is that we are primarily treating skin cancers. We are not primarily treating squamous cell carcinoma of the skin or melanoma; we are treating the skin of patients going through any type of cancer. Although many oncodermatologists feel comfortable with treating complex skin cancers, we are a different specialty. There is cutaneous oncology, which is the management of skin cancers, whether by a dermatologist or oncologist. And there is our specialty, oncodermatology, which manages the skin of patients with all types of cancer. Sometimes, these two different specialties will be conflated.
How would a patient know if they should visit an oncodermatologist during their treatment?
That decision is both patient- and oncologist-dependent. An oncodermatologist’s intention is to support patients during their cancer journey. Some patients do not need our services. Their skin is not being affected by their cancer care, so visiting an oncodermatologist may not be necessary. For other patients, their skin is very much affected, so seeing an oncodermatologist might be critical to allowing them to maintain their cancer therapy. In addition, seeing an oncodermatologist might be necessary to preserve a patient’s function. Therefore, it is critical for those populations to see an oncodermatologist.
Sometimes, there are preventative measures an oncodermatologist can take to avoid certain types of skin toxicities. Other times, we can help manage skin toxicities once they have already manifested.
Would patients with nonmelanoma skin cancer or melanoma on regimens containing pembrolizumab or cemiplimab need to visit an oncodermatologist?
These two agents, pembrolizumab and cemiplimab, are in a drug class called immunotherapies or immune checkpoint inhibitors. Those medications are designed to enhance the immune system to fight cancer. Essentially, they train your immune system. During that training process, your immune system may learn to attack other things, including the skin.
Skin side effects to immunotherapy, including pembrolizumab and cemiplimab, are very common. For some patients, those side effects manifest as an itch or simple rash. For others, it can develop into whole-body psoriasis. Others might even develop auto-immune skin diseases. Even though these medications are relatively new, oncodermatologists have significant experience evaluating and managing these rashes. Many oncodermatology therapies are quite effective and can allow patients to stay on treatment. The goal is always to allow patients to be treated for their skin issues while they are on their cancer therapy.
What are some common oncodermatology treatments?
Oncodermatology treatments are derived from the treatments used throughout dermatology. These include topical medications, light-based therapies, and systemic therapies, including both oral and injectable medications. When picking treatments within oncodermatology, the goal is to make sure that what we do is compatible with cancer care. We typically pick things that are very targeted. We also like to keep the immune system as intact as possible to allow the immune system to continue fighting the cancer. We also like to preserve the gut as much as possible. There is good data suggesting that preservation of the gut microbiota is associated with better outcomes in cancer care.
When considering treatments, whether topical or systemic agents, I like to tell my patients that we are as involved as they need us to be. Suppose they have a toxicity in the skin that is relatively mild. In that case, we do not need to give them a complicated or intensive regimen. If they have a more severe toxicity, then they might need several lines of therapy to help preserve their quality of life. That extra “homework” is sometimes reasonable to them because it allows them to keep their quality of life higher while continuing treatment.
What is a key takeaway you want people to know?
Everyone has a very individualized cancer journey. This journey spans everything from how their cancer is detected to how it affects them, what treatments are given for their cancer, and how they experience side effects, if any, from that cancer therapy. Because of how individualized everyone’s cancer journey is, it is critical to make personalized and individual decisions every step of the way. That includes how they want to manage side effects.
If things are important to you as a patient, they should be important to clinicians. I tell this to my patients: if it matters to you, then it matters to me. If it doesn’t matter to you, then I will let you know if it will impact your overall health. I will always let you know if something is going to be dangerous or if I think there is room for improvement. I will never push anything that would be an extra burden on an already taxing journey.

Timothy Dang, MD, is a Dermatologist and an Assistant Professor in the Department of Dermatology at the University of California San Diego School of Medicine. He joined the staff in August 2023. Dr. Dang practices general dermatology with special interests in cutaneous lymphoma and supportive oncodermatology, which is the management of dermatologic issues and toxicities that arise in the setting of cancer treatment. At the University of California San Diego School of Medicine, he trains medical students and residents. He received his medical degree from the Stanford University School of Medicine in Stanford, California. His residency was completed in dermatology at Harvard Medical School and Massachusetts General Hospital in Boston, Massachusetts. Dr. Dang was recently an author on “Basal Cell Carcinoma Formation Within a Spinal Cord Stimulator Surgical Scar: A Case Report.”
Recent Posts

Regeneron Announces Approval of Cemiplimab-rwlc for Adjuvant Treatment of Cutaneous Squamous-Cell Carcinoma with a High Risk of Recurrence After Surgery and Radiation
Preparing for Your First Oncology Visit: A Complete Guide for Skin Cancer Patients

Skin Cancer in Aging Veterans: Unique Risks & Considerations
The Genetics of Skin Cancer: Insights from Dr. Kenneth Tsai